Aesop’s fable about the blind men and an elephant is a story of a group of blind men who have never come across an elephant. To learn and imagine what the elephant is like, they each are given a body part to examine with their hands. Each blind man feels a different part of the elephant’s body, but only one part, such as the side or the tusk. The men then describe the elephant based on their brief experience with the animal. As one can imagine, the descriptions vary….
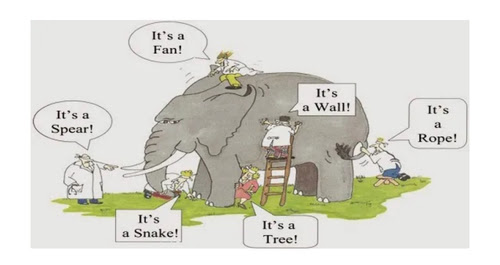 I found this fable to be representative of the struggle some have in our overly specialized healthcare system. We, as providers, are great at seeing the individual parts and knowing our specialty but this can be at the expense of patients being seen as a whole person. Sleep disordered breathing (SDB) is an underlying health risk that often goes unrecognized due to an under-appreciation for just how important quality sleep is to our mind and our body. Additionally, many can suffer from SDB without any audible indications like snoring.
I found this fable to be representative of the struggle some have in our overly specialized healthcare system. We, as providers, are great at seeing the individual parts and knowing our specialty but this can be at the expense of patients being seen as a whole person. Sleep disordered breathing (SDB) is an underlying health risk that often goes unrecognized due to an under-appreciation for just how important quality sleep is to our mind and our body. Additionally, many can suffer from SDB without any audible indications like snoring.
Part I of this series covered why it is so important to breathe through your nose. Part II is a deeper dive into what happens when our daily struggles to breathe properly impact the quality and quantity of sleep we are able to achieve. Part III will cover the implications on children who may suffer from struggles to breathe properly both day and night.
Sleep has three basic stages:
- Light or Core sleep is about 30-60% of a good night’s rest. This stage of sleep gets your body ready for the next phase, deep sleep…
- Deep sleep consumes about 15-30% of the total time sleeping. Eye movement has stopped, muscle movement slows and blood pressure decreases. This is when your body repairs damage from the day.
- REM sleep is considered the final stage of sleep and typically accounts for 20-30% of total sleep. Your body uses REM sleep to process new tasks, to repair neural connectivity and for emotional processing.
When breathing is obstructed or challenged during sleep, the brain goes into ‘fight for flight’ mode. Oxygen is needed for our existence. When the brain senses a struggle to collect sufficient air flow our brains will disrupt us into a lighter form of sleep. This happens so that muscles can contract and the body can move in an effort to open the airway. This may appear on the surface to be a minor issue but repetitive nights of poor sleep while struggling to get adequate oxygen flow can lead to a cascade of systemic health events, from high blood pressure and obesity to anxiety and depression.
Our bodies release adrenaline in a ‘fight or flight’ response to a reduction in oxygen and an increase in carbon dioxide, which causes stress both to the brain and the body. This sets off a cascade of stress hormone responses and can lead to increased cortisol levels, something often associated with elevated cardiovascular risks.
Decreased quantity and quality of sleep can also cause a reduction in the levels of the hormone leptin which is responsible for telling the brain that enough food has been consumed. In turn, the body increases levels of grehlin, the hormone that stimulates appetite. When we don’t sleep well or long enough, we tend to crave more carbohydrates and sugar. With our turn off mechanism destabilized, we can overconsume leading to the addition of unwanted pounds.
Imagine being repeatedly suffocated at night while you’re trying to sleep. A harsh visual, right??!! This is what happens when our airways become obstructed during our bodies time for rest and recovery. The physiological stress response can lead to feelings of anxiousness and depression. The fear of suffocation is primal and universal. The anxiety that this causes at night can carry over into our day making the simplest of tasks feel monumental or the smallest of infractions seem like the biggest crime.
As your dental health provider, I am trained to evaluate airways and oral indications of sleep disordered breathing. My staff and I have been treating patients with sleep apnea for more than a decade. It is only with recent study that I have become aware of the number of patients who may not snore but suffer from sleep disordered breathing, compromising their ability to get a good night’s rest allowing the body heal and restore. Yes, quiet sleepers can experience oxygen deprivation and making their diagnosis less common than those who snore.
If you think this is a condition you or a loved one may have, I look forward to discussing this with you at your next appointment. In the meantime, here is something you can try at home to evaluate your sleep. Many companies now make monitoring watches and rings that can prepare a sleep report with information about your amount of time in each sleep stage, your oxygen saturation levels, your heartrate and your breathing rate. You can check out these products online: here, here and here are just a few options.
In closing, I want to thank you for the opportunity to care for you. It is an honor to be entrusted as your dental provider and I do not take my role lightly. I look forward to seeing you at your next visit and to helping you achieve health goals.
Gratefully,
Jessica
